Galapagos of neuroscience
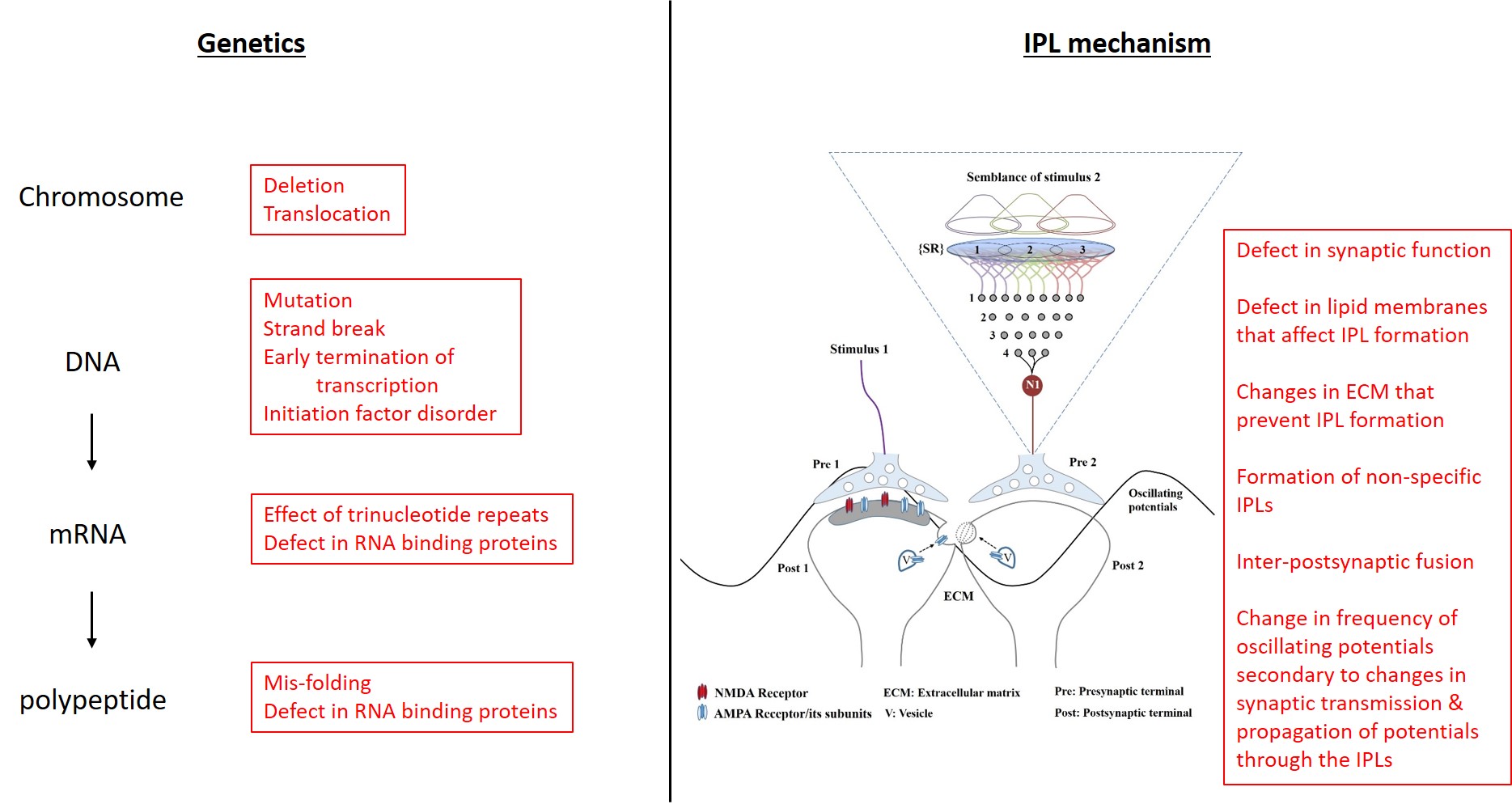
Figure 1. Disease conditions of different systems can be and should be explained in terms of “change of function” states of the normal operations of those systems. Only when we understand how a system operates, we can explain the causes of different diseases of that system in an inter-connectable manner that makes sense. On the left is a general outline of genomic function and how defects at different levels cause its different disorders. On the right side is the derived inter-postsynaptic functional LINK (IPL) mechanism of nervous system operations and the potential defects that can arise at its different levels. Note that vesicle (V) exocytosis at the inter-spine locations leads to membrane reorganization that can promote IPL formation. Also note that defects in the IPL formation can lead to IPL fusion (see the figure 8 in FAQ section of this website). What is not shown in the figure is the observation that dopamine leads to the enlargement of spines, which can facilitate IPL formation. Our job is to examine all the nervous system disorders to find whether the disease processes can be explained in terms of the defects of the derived normal IPL mechanism. For details of the figure, please see the figure legends of figures 6 and 8 in the FAQ section of this website.
In this
1. Huntington's
Disease: Early disease symptoms include slight memory problems,
clumsiness, depression, mood swings such as irritability and erratic
behavior. Later, the patient starts developing involuntary, hyperkinetic
movements called chorea (uncontrollable, graceful, excessive movements
of limbs similar to that of performing a dance). At advanced stages,
chorea settles down and the patient develops severe parkinsonian
features.
Explanations based on IPL formation:
Basic explanation for the
pathology: Excessive dopamine leads to spine expansion that lead to the
formation of non-specific IPLs and eventually IPL fusion that leads to
spine loss and eventually neuronal death. These changes are expected to
be formed at the locations where dopaminergic inputs arrive and
eventually cause expansion of spines of synapses having other
neurotransmitters. Experiments that added dopamine artificially to
synaptic regions in both striatum and nucleus acccumbens (O'Donnell &
Grace, 1993; Onn and Grace, 1994) have shown fusion between neurons as
evidenced by dye diffusion between neighbouring neurons. Based on
semblance hypothesis, IPL formation is taking place between spines that
belong to different neurons as a default mechanism and that excessive
dopamine is generating IPL fusion that allows dye to transfer between
the neurons whose spines undergo IPL fusion. Note that IPL fusion is at
the far end of the spectrum of different IPLs (Figure 8 in the FAQ
section of this website; Vadakkan, 2016a).
Subcortical dementia:
Non-specific IPLs cause dilution of specific semblances, expected to form
during retrieval of a specific memory, with non-specific semblances.
This results in memory lapses.
Psychiatric features:
Formation of non-specific IPLs can lead to hallucinations (Vadakkan,
2012a).
Hyperkinetic movements
(chorea): Formation of excessive number of IPLs leads to excessive
activation of motor units. When regulatory pathways are brought in
place, this can generate excessive graceful movements of chorea.
Parkinsonian features
during the last stages: IPL fusion leads to spine loss. Large number of
spines on the medium spiny neurons undergo IPL fusion, which leads to
spine loss and eventual loss of these neurons. This eventually reduces
the number of medium spiny neurons and their spines that can form IPLs,
which will have an equivalent effect of having a reduced amount of
dopamine for facilitating rapid IPL formation as expected in Parkinson's
disease (Vadakkan, 2016b).
Later stage shows loss of
volume of the caudate head in brain imaging: This can be explained in
terms of neuronal loss secondary to IPL fusion changes.
Patients have reduced
saccadic movements of the eyeballs. It will be possible to find out the
exact location where excessive IPL formation leads to this sign, which
is routinely used to diagnose this disorder at an early stage.
The abnormal protein, namely Huntingtin, produced in Huntington's
disease is a component of vesicle membranes. This may have additional
influence on IPL fusion.
Extreme delta brush is an
EEG finding: There are large wavy patterns that have excessive
horizontal component in the waveforms. It will be possible to explain
this finding in terms of excessive number of IPLs that form large islets
of inter-LINKed spines in the cortices.
Westphal variant of
Huntington's disease starts at a young age. The main features include is
akinetic rigidity, seizures (Vadakkan, 2016c) and myoclonus. These
symptoms can also be explained in terms of the formation of excessive
IPLs.
Interconnected findings that provide support for the IPL mechanism include the following:
1) Excessive dopamine leads to excessive enlargement of spines, which leads to the formation of non-specific IPLs.
2) IPL fusion resulting in memory problems,
hyperkinetic movements and hallucinations.
2. Parkinson's disease:
Disease
symptoms include tremor, rigidity bradykinesia and postural instability.
Later cognitive defects, dyskinesia and hallucinations develop.
What is currently known? It is caused by damage to the substantia nigra
(pars compacta) neurons that release dopamine at their axonal terminals
that synapse with medium spiny neurons (named due to the relatively
large number of spines on them) of the basal ganglia. Dopamine activates
both direct and indirect pathways in the basal ganglia to regulate the
thalamic output to the upper motor neurons of the motor cortex to
smoothen the motor actions. L-DOPA is used in the treatment. It is
converted to dopamine and binds to the dopamine receptors. It then leads
to both activation of the direct pathway and inhibition of an indirect
pathway that together smoothen the motor actions. The effect of a fixed
dose of L-DOPA reduces gradually. As the disease progresses, patients
will require a
higher dose of the drug at more
frequent intervals to have the same initial effect. Eventually, even
with high doses of L-DOPA the disease become uncontrollable. Moreover,
side effect of L-DOPA limits usage of this medication beyond a certain
amount. After a few years, patient gets mild cognitive impairment. At
advanced stages, patients suffer from more cognitive problems and often
get hallucinations.
Explanations based on IPL formation:
Basic explanation for the
normal actions: Normal concentration of dopamine reaching the
dopaminergic synapses leads to the enlargement of spines of medium spiny
neurons and generates IPLs (without causing IPL fusion) that facilitates
activation of thalamic outputs to the motor cortex. This helps to make
smooth motor movements.
Basic explanation for the
pathology: Since the initial use of L-DOPA just before 1970, every
Parkinson's disease patient is using dopaminergic medications. This has
affected the natural history of the disease that we observe currently.
Dopamine leads to the enlargement of the spines. Artificial increase in
dopamine levels by the administration of L-DOPA is different from the
physiological concentration of dopamine released to the dopaminergic
synapses. Furthermore, it is not known how different factors can
influence the consequences of spine enlargement by dopamine. It is
probable that dopamine eventually leads to fusion between the spines
that belong to different medium spiny neurons and can lead to loss of
spines. The factors predisposing to inter-spine fusion include changes
in lipid membrane composition, lack of proteins that can stabilize the
inter-spine hemifusion stage of fusion, etc. At advanced stages, spine
fusion can eventually result in spread of pathology to the dopaminergic
presynaptic terminals that synapse to the medium spiny neurons. Based on
the explanations by the IPL mechanism, in addition to supplementing
dopamine, it is necessary to find methods to stabilize the IPLs to
prevent them from progressing to the IPL fusion stage.
Memory problems: During the initial stages, lack of dopamine affects
both the motor actions and cognition. Later, administration of dopamine
result in enlargement spines and IPL fusion that can lead to loss of
spines and neurons.
Bradykinesia: Due to a
lack of dopamine, the net output from the direct and indirect pathways
to the thalamus is reduced.
Hallucinations: At the
advanced stages of the disease when the patients need more dopamine for
maintaining movement, they suffer from hallucinations. Treatment with
dopamine leads to the enlargement of non-specific sets of spines that
can lead to the formation of non-specific IPLs, which in turn can induce
non-specific semblances responsible for hallucinations.
Interconnected findings
that provide support for the IPL mechanism:
1) Parkinsonian features
during the last stages of Huntington’s disease: Since a large number of
spines of medium spiny neurons in Huntington’s disease undergo fusion,
there will be both losses of these spines and their neurons. This
produces symptoms of hypokinetic movements of Parkinson’s disease
resulting from the reduced amount of dopamine that can facilitate IPL
formation (Vadakkan 2016b).
2) The increased movements causing chorea is most commonly seen in patients with Parkinson's disease who are taking neuroleptic medications that are dopamine receptor D2 blockers. When D2 receptors are blocked, whatever dopamine is available from substantia nigra pars compacta binds to the D1 receptors and results in unopposed activation of the direct pathway leading to hyperkinetic movements of chorea. This can lead to IPL fusion between spines belonging to different neurons. The end result will be similar to that of Huntingon's disease.
3. Headache Pains
Therapeutic agents
effective in unrelated neurological and psychiatric disorders alleviate
different types of headaches
First, there are large number of distinct
headache pains that has their own unique features. Secondly, medications
having opposite actions such as a) dopaminergic and dopamine antagonists
b) those that increase and decrease oxygenation and/or circulation are
used to alleviate different headaches, indicating that there is an
optimal state for a mechanism whose changes to either side generate
internal sensations of pain. Thirdly, pain is sensed during a conscious
state indicating that the mechanism of internal sensation of pain has a
deep relationship with consciousness. Fourthly, medications used in
unrelated neurological and psychiatric disorders are used to alleviate
distinct types of headaches, indicating that there is a deep underlying
common mechanism that is being reversed by these medications.
Demonstration of the latter is essential to confirm the identification of the
mechanism of both pain and neurological and psychiatric disorders where
these pharmaceutical agents are effective. IPL mechanism satisfies these
requirements.
Therapeutic agents act at different targets along
the axis of the mechanism as explained below.
1. Reducing consciousness: By forming
large number of non-specific IPLs, general anesthetics alter
conformation of C-semblance altering consciousness (Vadakkan, 2010;
2015b). When C-semblance is altered, p-semblance cannot be formed. This
explains a mechanism how anesthetic agents prevent internal sensation of
pain.
2.
Altering sensory inputs: Botulinum toxin, local anesthetic agents,
and plastic surgery are used for treating different types of pain (Becker,
2020; Robbins et al., 2014; Kung et al., 2011). If sensory inputs act as
noxious stimuli, then removing these input can alleviate pain.
Furthermore,
qualia of
internal sensation take place by retrograde extrapolation from the
inter-LINKed spine towards all the sensory receptors (Vadakkan, 2013).
When these sensory receptors are removed by plastic surgery, then it can
eventually alter the qualia of pain.
4. Altering dendritic spine size
a.
Increasing
spine size: Dopamine is known to increase spines size (Yagishita et al.,
2014). Dihydroergotamine is a dopamine agonist that has been used for
treating refractory headaches (Nagy et al., 2011). It is expected
to promote formation non-specific IPLs in the cortex and alter
conformation of p-semblance.
b. Decreasing spine size
by blockers of dopamine action: Chlorpromazine is a dopamine antagonist
and is used in acute headaches (Hodgson et al., 2021) and also to break
the cycle of
headaches. It is expected to reduce the size of spines and that will
reverse large number of IPLs. Chlorpromazine was used routinely to treat
psychosis until the arrival of newer medications. It can be explained by
its ability to reverse large number of non-specific IPLs present in
people with psychotic disorders (Vadakkan, 2012).
5. Altering IPL formation: Altering the number of IPLs by increasing oxygenation
1.
Oxygen is used as a
treatment for cluster headache (Cohen et al.,
2009). The quick relief of this excruciating pain can be explained in
terms of reduction in the number of IPLs responsible for inducing
p-semblance. Evidence for this comes from indirect findings that need to
be verified. a) Modified Golgi stain showed reticulate pattern of
connections between neurons. When this was modified by Ramon Cajal using
strong oxidizing agents spread of stain was limited to dendritic spines
(postsynaptic terminals). The Golgi stain is formed by the black color
of metallic silver when silver nitrate is reduced (opposite of
oxidation). Additional oxidizing agents used in the reaction mixture
decrease the ability of tissue to reduce silver nitrate to silver and
thereby restrict the spread of the reaction beyond the spines (Vadakkan,
2021c). Also note
that presynaptic terminal is most resistant to Golgi stain. Hence, it
can be inferred that the spread of Golgi stain to form a reticulated
pattern when oxidizing agents are decreased most probably takes place
through a non-trans-synaptic route. If all the above are true, then a
reasonable inference that can be drawn is that maintenance of IPLs is an
oxidation-state dependent process. This can be verified by conducting
experiments. b) Rapid irreversible brain death due to lack of oxygen
also prompts further investigations. If the inferences from modified
Golgi staining can be verified, then it means that any lack of oxygen
will lead to IPL fusion very quickly. The inference that IPL fusion is
prevented by an adaptation (Vadakkan, 2020) also supports this view.
This can explain rapid irreversible brain death due to lack of oxygen.
The incentive in studying this is that once confirmed, it is possible to
use intravenous oxidizing agents to prevent IPL fusion in acute anoxic
conditions and prevent brain death.
2.
Vasodilatation: Propranolol can increase blood flow that can promote
oxidation state dependent alteration in the number of IPLs similar to
the effect of oxygen. Since propranolol is the most lipophilic beta
blocker, it may interact with membrane lipid bilayers and can cause
changes in number of IPLs.
3.
Anti-seizure medications:
Topiramate is an anti-seizure medication that is expected to operate by
blocking rapid chain reaction of IPLs (Vadakkan,
2016c). A similar effect can reduce migraine headaches. Similar action of
anti-seizure mediation carbamazepine can explain how it is effective in
alleviating trigeminal neuralgia, pain of herpes zoster, and neuropathic
pain.
4.
Sumatriptan cause vasoconstriction and reduce headache caused by
vasodilation. By reducing the flow of blood, sumatriptan reduces
available oxygen, which in turn alters the number of IPLs to change the
conformation of p-semblance.
c) Migraine type of headache seldom occurs after the age of 45. This is possibly due to slow spread of generation of IPLs due to changes in the ECM.
Special cases of pain
In summary, IPL mechanism provides a common shared mechanism that can explain how medications with disparate actions are effective in headache pains and how they are effective in alleviating symptoms of unrelated neurological and psychiatric disorders. These are testable findings that can be verified.
------------------------------------------------------------------------------------------------------------------
Following
is an expanding
list of findings from
different neurological and psychiatric disorders that can be
examined for their suitablity for explanations
in terms of IPL formation and function. I hope to provide those
explanations in the due course. You can reach those explanations by
imagination based on the logic applied to explain several disease
conditions.
Seizures
(see Vadakkan, 2016c)
1.
Juvenile
Myoclonic Epilepsy - Generalized tonic clonic seizures provoked by sleep
deprivation. Childhood absence epilepsy – Children outgrow these
seizures
2.
Juvenile absence
seizures – Require life-long treatment
3.
Eye deviation at
the onset of seizure
4.
Post-ictal
aphasia shows that seizure lateralize to dominant hemisphere
5.
Short-acting
benzodiazepines become anesthetics. Clonazepam is useful for myoclonic,
absence and partial seizures. Lorazepam is useful for status
epilepticus. Midazolam (shortest life) is an anesthetic agent used in
status epilepticus. Does lipid solubility increase from clonazepam to
midazolam? Note that midazolam become much more lipid soluble at
physiological pH.
6.
One of the
effective treatment modalities of certain types of seizures is multiple
sub-pial resections. It usually reduces the intensity of seizures.
During this procedure, any horizontal connections (IPLs) get severed to
stop spread of synchronous seizure activity.
7.
Frontal lobe
seizure has Jacksonian march
8.
Automatisms are
involuntary complex motor activity during impaired consciousness. They
can occur with complex partial or absence seizures.
9. Early onset
benign childhood occipital epilepsy (Panayiotopoulos syndrome) has
visual seizures – elementary or complex visual hallucinations,
amaurosis, illusions (e. g. metamorphopsia), which are experience
usually during wakefulness. Inter-ictal EEG has nearly continuous bursts
or trains of high-voltage rhythmic occipital spikes and spike wave
complexes at a frequency of 1-3 Hz localized to uni or bilateral
occipital cortices with normal background activity. It increases during
non-REM sleep and disappears when eyes are opened. Late onset benign
childhood occipital epilepsy (Gestault) – Visual hallucinations are
often followed by migraine headache.
10.
Myoclonic seizure
originate from different locations
a: Cortical reflex
myoclonus: discharge from sensorimotor cortex
b: Reticular
reflex myoclonus: discharge from brainstem reticular formation
c: Primary
generalized epileptic myoclonus: diffuse bursts of polyspike & wave or
spike & wave
d:
Non-epileptic myoclonus: most common
11.
Seizure is seen
in SCA 7, SCA10 & DRPLA
12.
Valproic acid
causes more cognitive defects in seizures patients – matches with the
idea that it reduces IPLs (Meador et a., 2009)
13.
VPA increase IPLs
in some locations and decreased IPLs in other locations
14.
Impact seizure is
the immediate post-traumatic seizure
15.
TCA is an
anti-seizure medication – It is likely by IPL mechanism
16.
Landau-Kleffner
syndrome – Seizures and Language defects
19. Some seizures are responsive to B6 vitamin.
20 HSV infection cause PLEDS, periodic
slow wave complexes and diffuse slowing
Encephalopathies
Hypertensive encephalopathy –
symptoms aphasia, hemiparesis – seen in cyclosporine neurotoxicity due
to thrombocytopenia – possibly also has IPL fusion as the basic
causative pathology.
Methanol cause encephalopathy.
Long-term effect is Parkinsonism – Likely causing IPL fusion and lead to
spine loss
& neuronal death.
Hypoxic Ischemic
Encephalopathy (HIE): Ischemia cause release of phospholipases – free fatty
acids are released from neuronal membranes (Collard & Gellman, 2001)
Cytotoxic edema is seen
viral infections of the brain parenchyma. One possible explanation is
that viral fusion proteins can lead to cytoplasmic content mixing that
can lead to, spine loss & neuronal swelling, responsible for cytotoxic
edema
Myoclonus
1. Post anoxic myoclonus – is
an action myoclonus – this is almost always associated with cerebellar
ataxia. Not inhibited by Purkinji outputs. Often, it is a self-limited
condition.
Head Injury
Concussion: Acute
symptoms include headache, confusion, amnesia, dizziness, unsteadiness.
Signs include vacant starring, confusion, disorientation, memory
disturbances, ataxia, incoordination, slurred speech, & behavioral
disturbances.
There are several findings in the nervous system disease from where information can be taken to synthesize a mechanism for internal sensation of depression.
Antidepressant toxicity generarlly cause hallucinations, tremor, myoclonus, & seizures.
SSRIs can cause hyperkinetic movement disorders. Is it because of increased number of IPLs?
Dementia in metachromatic leukodystrophy
Abetalipoprotenemia has acanthocytosis – Is it possible to find a membrane defect in both acanthocytosis and dementia in neuroacanthocytosis?
In MSA, there is atrophy of pons and
cerebellum. It is necessary to examine how cells are lost in these
areas. Is there any evidence for IPL fusion
Several studies have shown involvement of the cortex in this disease.
Stroke
Following a stroke affecting the sensoroy cortex, some patients recover from defects in sensations of touch, pain & temperature. However, they still can have significant impairments in two-point discrimination & proprioception. It may mean that some cortical sensations are the result of secondary or tertiary conformations of semblances responsible for primary sensations.
Hypoxic damage
Certain areas of the brain thought to have increased oxidative phosphorylation such as basal ganglia are more prone to hypoxic damage. In addition to its role in oxidative phosphorylation, oxygen can exert its role an oxidising agent to reverse IPLs formed. In the absence of oxygen, IPL fusion can occur at these locations and can lead to spine loss and neuronal death. It is necessary to study whether these regions are rich in spiny neurons, where spines undergo rapid IPL formation and reversal for its functions.
Hallucinations
Both Cogan’s syndrome and
Charles Bonnet syndrome have reduced vision. Patients
with both these syndromes hallucinate. Is it because the system has IPLs that get reactivated by
some mechanism?
Heredodegenarative
disorders: has schizophrenia like psychosis. At ages between 40 & 60, it
causes dementia and Parkinsonism. Dementia is primarily subcortical.
MAO inhibitor selegiline
cause hallucination, vivid dreams, insomnia, dyskinesia, & depression
Viruses release fusion proteins that allow them to enter into cells and also exit from the cells after multiplication. Since IPL mechanism involves initial stages of fusion, neurological and psychiatric findings in these disorders can have direct relationships.
SSPE: a neurodegenerative disorder occurs after nearly 5-10 years. It has 4 phases 1) problems with behavior & cognition, 2) myoclonus, 3) reduced IQ, myoclonus, speech, 4) choreoathetosis, bradykinesia & rigidity.
Interconnected findings
Cortical
spreading depression in migraine; Jacksonian march in seizure.
Others:
1.
Porphyria -
Psychiatric symptoms, Abdominal pain.
Porphyria also cause anxiety, insomnia,
depression, hallucination, and paranoia.
2.
DRPLA onset
before age 20: Usually PME with seizures, dementia, ataxia and
myoclonus. If onset is after age 20, ataxia, dementia, and
choreoathetosis. All these findings can be explained in terms of changes
in IPL mechanism.
3. Hypercalcemia
patients have severe water deficit. So it can reduce water content of
the ECM. It can cause formation of large number of non-specific IPLs.
This can explain confusion, weakness, & pseudo-dementia.
4. Posterior
reversible encephalopathy syndrome
5. Sodium
oxyabate is an anesthetic agent – so formation of non-specific IPLs can
induce a state of reduced consciousness.
6. ALS – has laterally spreading sclerosis and
it is a pure denervation (no axonal or demyelination)?
7.
Some of the
subfornical organ (SFO)/ organum
vasculosum of the lamina terminalis (OVLT) neurons are osmosensitive.
Their firing rate increases in response to increases in the tonicity of
the extracellular fluid (Zimmerman et al., 2017).
ECM changes is likely leading to generation
of new IPLs that generates internal sensation of taste and trigger
firing of downstream neurons.
12.
NCL: features include seizures, regression (could be possibly due to IPL
fusion), blindness & psychiatric features
14.
Gaucher’s disease
patients have seizures, memory problems, spasticity, ataxia,
&
15.
Abbreviations
ALS: Amyotrophic lateral sclerosis
CJD: Creutzfeldt-Jakob disease
CO: Carbon monoxide
DRPLA: Dentatorubral-pallidoluysian atrophy
GPi: Globus pallidus interna
PME: Progressive myoclonic epilepsy
PRES: Posterior reversible encephalopathy
syndrome
SCA: Spinocerebellar strophy
References
Akerman
S, Goadsby PJ (2005) Topiramate inhibits cortical spreading depression
in rat and cat: impact in migraine aura. Neuroreport. 16(12):1383–1387. PubMed
Ayata C, Lauritzen M (2015) Spreading
Depression, Spreading Depolarizations, and the Cerebral
Vasculature. Physiol Rev. 95(3):953–993. Article
Becker WJ
(2020) Botulinum
Toxin in the Treatment of Headache. Toxins
(Basel). 12(12):803. Article
Calabresi et al., (2014) Direct and
indirect pathways of basal ganglia: a critical reappraisal. Nature
Neuroscience 17(8):1022-1030 Article
Cohen A, Burns B, Goadsby PJ (2009)
High-flow oxygen for treatment of cluster headache: a randomized
trial. JAMA. 302(22):2451–2457. Article
Collard & Gellman (2001) Pathophysiology,
clinical manifestations, and prevention of ischemia-reperfusion injury.
Anesthesiology. 94: 1133
Dreier JP, Reiffurth C (2015) The
stroke-migraine depolarization continuum. Neuron. 86(4):902–922. Article
Hodgson SE,
Harding AM, Bourke EM, Taylor DM, Greene SL (2021) A
prospective, randomized, double-blind trial of intravenous
chlorpromazine versus intravenous prochlorperazine for the treatment of
acute migraine in adults presenting to the emergency department. Headache. 61(4):603-611. Article
Karnani MM,
Agetsuma M, Yuste R (2014) A blanket of
inhibition: functional inferences from dense inhibitory connectivity. Curr
Opin Neurobiol. 26:96-102. Article
Koyama T, Kato K, Tanaka YZ, Mikami A
(2001) Anterior cingulate activity during pain-avoidance and reward
tasks in monkeys. Neurosci
Res. 39(4):421–430. Article
Kung TA,
Guyuron B, Cederna PS (2011) Migraine surgery:
a plastic surgery solution for refractory migraine headache. Plast
Reconstr Surg. 127(1):181–189. Article
Meador et al., (2009) Cognitive function
at 3 years of age after fetal exposure to antiepileptic drugs. N Engl J
Med. 360(16):1597-605. Article
Nagy AJ,
Gandhi S, Bhola R, Goadsby PJ (2011) Intravenous dihydroergotamine for
inpatient management of refractory primary
headaches. Neurology. 77:1827–1832. Article
O'Donnell P, Grace AA (1993) Dopaminergic
modulation of dye coupling between neurons in the core and shell regions
of the NAc. J Neurosci 13(8): 3456-3471 Article
Onn SP, Grace AA (1994) Dye coupling
between rat striatal neurons recorded in vivo: compartmental
organization and modulation by dopamine. J Neurophysiol 71(5):
1917-1934. Article
Piovesan EJ, Kowacs PA, Tatsui CE, Lange
MC, Ribas LC, Werneck LC (2001) Referred pain after painful stimulation
of the greater occipital nerve in humans: evidence of convergence of
cervical afferences on trigeminal nuclei. Cephalalgia. 21(2):107–109. Article
Robbins MS,
Kuruvilla D, Blumenfeld A, Charleston L 4th, Sorrell M, Robertson CE,
Grosberg BM, Bender SD, Napchan U, Ashkenazi A (2014) Trigger
point injections for headache disorders: expert consensus methodology
and narrative review. Headache. 54(9):1441–59. Article
Saldanha IJ, Cao W, Bhuma MR, Konnyu KJ,
Adam GP, Mehta S, Zullo AR, Chen KK, Roth JL, Balk
EM (2021) Management
of primary headaches during pregnancy, postpartum, and breastfeeding: A
systematic review. Headache. 61(1):11–43. Article
Unekawa M, Tomita Y, Toriumi H, Suzuki N
(2012) Suppressive effect of chronic peroral topiramate on
potassium-induced cortical spreading depression in rats. Cephalalgia. 32(7):518–527. Article
Vadakkan KI
(2010) Framework of consciousness from semblance of activity at
functionally LINKed postsynaptic membranes. Front
Psychol. 1:168. Article
Vadakkan KI (2012)A structure function mechanism for
schizhophrenia. Front. Psychiatry. Article
Vadakkan KI
(2013) A
supplementary circuit rule-set for the neuronal wiring. Front
Hum Neurosci. 7:170. Article
Vadakkan KI
(2015a) A
framework for the first-person internal sensation of visual perception
in mammals and a comparable circuitry for olfactory perception in
Drosophila. Springerplus. 4:833. Article
Vadakkan KI (2015b) A pressure-reversible cellular mechanism of
general anesthetics capable of altering a possible mechanism for
consciousness. SpringerPlus. 4:485. Article
Vadakkan KI
(2016a) The functional role of all postsynaptic potentials examined from
a first-person frame of reference. Reviews in the Neurosciences.
27(2):159-84. Article
Vadakkan KI (2016b)
Neurodegenerative disorders share common features of "loss of function"
states of a proposed mechanism of nervous system functions. Biomedicine
and Pharmacotherapy. Article
Vadakkan KI (2016c)
Rapid chain-generation of inter-postsynaptic functional LINKs can
trigger seizure generation: Evidence for potential interconnections from
pathology to behavior. Epilepsy & Behavior. 59: 28-41. Article
Vadakkan KI
(2020) A
derived mechanism of nervous system functions explains aging-related
neurodegeneration as a gradual loss of an evolutionary adaptation. Curr
Aging Sci. 13(2):136-152. Article
Vadakkan K.I (2021a) Neurological
disorders of COVID-19 can be explained in terms of both "loss and gain
of function" states of a solution for the nervous system. Brain
Circulation. Article
Vadakkan K.I
(2021b) Framework for internal sensation of pleasure using constraints
from disparate findings in nucleus accumbens. World Journal of
Psychiatry. Article.
Vadakkan KI (2021c) Golgi staining of
neurons: Oxidation-state dependent spread of chemical reaction
identifies a testable property of the connectome. OSF
Preprints
Trotta L,
Weigt K, Schinnerling K, Geelhaar-Karsch A, Oelkers G, Biagi F, Corazza
GR, Allers K, Schneider T, Erben U, Moos V (2017) Peripheral
T-Cell Reactivity to Heat Shock Protein 70 and Its Cofactor GrpE from
Tropheryma whipplei Is Reduced in Patients with Classical Whipple's
Disease. Infect
Immun. 85(8):e00363-17.
Yagishita S, Hayashi-Takagi A,
Ellis-Davies GC, Urakubo H, Ishii S, Kasai H (2014) A critical time
window for dopamine actions on the structural plasticity of dendritic
spines. Science. 345:1616–1620. Article
Zimmerman CA, Leib DE, Knight ZA (2017)
Neural circuits underlying thirst and fluid homeostasis. Nat Rev
Neurosci. 18(8):459-469. Article